This is the fourth of five articles on medical cannabis and its use as a peripheral neuropathy treatment.
Benefits and Effects of Medical Cannabis for Treating Peripheral Neuropathy
by Dr. Rosemary Mazanet
Benefits of Medical Cannabis
Although CBD and THC act differently in the body, they seem to have many of the same medical benefits. Unfortunately, most of this evidence comes from animals, since very few studies on cannabis have been carried out in human patients. The important result from preclinical animal models for neuropathy patients is that in rats, THC and CBD have been shown to be neuroprotective antioxidants. Many of the medical benefits of cannabis are attributed to the CBD content, particularly the strong anti-inflammatory and anti-seizure properties. As mentioned early, through plant genetics, marijuana can be grown richer in THC or CBD, allows growers and patients to select strain types that will give them very specific effects. That said, many patients find that the results they experience with the “entourage” effect is different from what they expected before using medical cannabis.
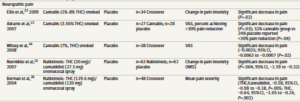
A recent publication by Hill et al, reports the randomized trials of cannabis for neuropathic pain. They interrogated the MEDLINE scientific publication database through March 2015, and found five placebo-controlled trials that investigated neuropathic pain. Unfortunately, these small trials all studied a different ratio and strength of THC:CBD, ingested in different fashions. Regardless, the evidence seems to indicate that Cannabis does reduce neuropathic pain in patients when they are blinded to the treatment (placebo or cannabis), the strictest criterion for clinical trial study.
Effects of Cannabis
While many psychoactive drugs clearly fall into the category of stimulant, depressant, or hallucinogen, cannabis hybrids exhibits a mix of all properties. Some of the short-term physical effects of cannabis use include increased heart rate, dry mouth, reddening of the eyes, muscle relaxation and a sensation of cold or hot.
Patients should treat marijuana for medical use like they would any prescription and avoid operating a motor vehicle or heavy machinery, performing child or elder care, and making important decisions while under treatment.
Appetite
The feeling of increased appetite following the use of cannabis has been documented for hundreds of years, and is known colloquially as “the munchies.” The activation of cannabinoid receptors in the hypothalamus is responsible for maintaining and or increasing food intake. For many of the conditions where medical cannabis is used, the increased food enjoyment and intake has been seen as a beneficial effect.
Side Effects
Anxiety and paranoia are the most commonly reported side effect of smoking marijuana with a high THC content. Other effects may include a general alteration of conscious perception, euphoria, feelings of well-being, relaxation or stress reduction, increased sensuality, increased awareness of sensation, increased libido, and creativity. Cannabis also produces many subjective effects, such as greater enjoyment of food taste and aroma, an enhanced enjoyment of music and comedy, and marked distortions in the perception of time and space. With very high doses, THC can induce auditory and visual hallucinations. THC should be used only under the care of a physician by anyone with a mental health history. In starting out using medical cannabis, users may be better off using cannabis with higher levels of CBD to reduce potential side effects.
As mentioned earlier, there are short-term physical effects of cannabis that include increased heart rate, dry mouth, reddening of the eyes, muscle relaxation and a sensation of cold or hot.
Although cannabis is not addictive in the classic sense, it can result in patient dependence and cannabis “use disorder” is defined as a medical diagnosis in the fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Both CBD and THC have been found to present no risk of lethal overdose. Opioid receptors are present in areas of the brain that control breathing and ingestion of excessive narcotics can cause a person to stop breathing. Unlike opioid receptors, cannabinoid receptors are not located in these brain stem areas. Marijuana cannot cause someone to stop breathing, no matter how much they ingest.
Memory
Reliable studies on cannabis and memory are hindered by small sample sizes, confounding drug use, and other factors, however it is agreed generally that cannabis use does affect perception, but does not cause permanent brain damage in adults. Researchers looking at data from 15 previously published controlled studies involving 704 long-term adult cannabis users and 484 nonusers concluded that long-term cannabis use was only marginally harmful on the memory and learning.
Very heavy use of marijuana is associated with decrements in neurocognitive performance, and any use of marijuana in children and adolescents is to be avoided except in the cases of supervised treatment for severe epilepsy.
Duration of Effects
Peak levels of cannabis-associated intoxication occur approximately 30 minutes after smoking. The total short-term duration of cannabis effects when smoked is based on the potency, method of smoking (vape) and how much is smoked. Any acute effects that accompany cannabis use usually abate after 6 hours.
When taken orally (in the form of capsules, food or drink), the effects take longer to manifest initially, and generally last longer, typically for 4–10 hours after consumption. Taking marijuana in the form of edibles can have unpredictable effects, since they are delayed and thus harder to predict.
Because cannabinoids are lipophilic (fat soluble) compounds that are easily stored in fat, they have a long “elimination half-life” or time they can still be detected in the body. Cannabis and its and related compounds can usually be detectable in the urine or blood for 3 days after episodic use, and up to 10 days with frequent use. Long-term users can produce positive tests for two to three months after ceasing cannabis use.
This is the fourth in a series of five articles on medical cannabis by Dr. Mazanet for the Foundation for Peripheral Neuropathy:
- The Status of Legalized Medical Marijuana and What is Dispensed
- The History of Cannabis Use
- How Does Cannabis Work?
- The Benefits and Effects of Medical Cannabis
- How to Use Medical Cannabis
About the author: Dr. Rosemary Mazanet, MD, PhD, was trained in Internal Medicine (Brigham and Women’s Hospital, Boston) and Medical Oncology (Dana Farber Cancer Institute, Boston), and has been active in the Biotechnology community for the last 30 years. Currently she is involved in strategic drug development and is the head of the Scientific Advisory Board for Columbia Care, Inc, a company that grows and dispenses legal medical cannabis in 9 states.

Ohhh I just found the first 4 articles…Thank you!